Slow breathing is a highly effective yet overlooked therapy for diabetes.
It profoundly changed my life with diabetes, leading me to spend the past 5 years trying to understand it and share it with others.
I’ve found that it’s not going to fix everything (of course). It may not even impact your blood sugars. But, without question, two things it will do are improve your heart health and your quality of life.
And it’s available anytime, anywhere (no pre-authorization required).
I think it’s a no-brainer for better health, and I hope this article inspires you to give it a try.
What is Slow Breathing? (and why was 6 breaths/minute in the title?)
Slow breathing is broadly defined as breathing at a rate of less than 10 breaths per minute. More specifically, it usually refers to breathing at a rate of about 4.5 to 7 breaths per minute.
And even more specifically, almost every study on slow breathing and diabetes has used 6 breaths per minute. And they’ve found some pretty remarkable things.
But before we get to that, let’s take a quick look at the breath-heart connection.
Understanding the Breath-Heart Connection: Respiratory Sinus Arrhythmia and Heart Rate Variability
When we inhale, our heart rate increases. When we exhale, it decreases (if you’d like more details, here’s a blog I wrote for ResBiotic that explains it fully). This is known as respiratory sinus arrhythmia (RSA).
RSA is one of the underlying principles of heart rate variability (HRV). Generally speaking, HRV is the beat-to-beat time variability of heart rate. Research shows that higher HRV indicates a more balanced nervous system and better cardiovascular health. For these reasons, higher HRV is associated with a better quality of life.
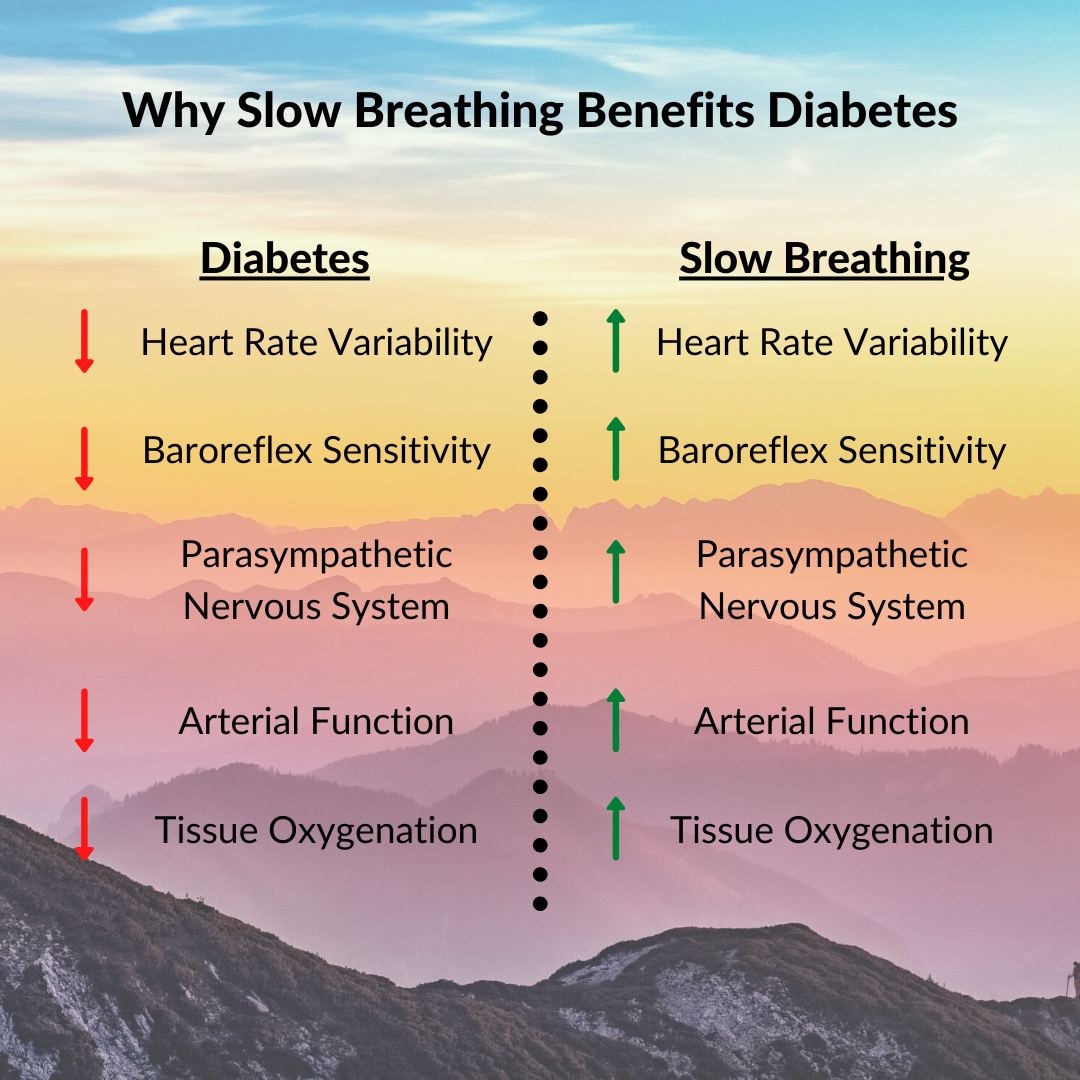
And it turns out that people with diabetes typically have worse HRV than non-diabetics. (A negative side-effect of researching diabetes is that it reminds me of everything it adversely affects. However, it’s also encouraging to find simple tools like breathing that can help (not fix) some of the problems).
HRV is Reduced in Diabetes
A 2018 meta-analysis found that patients with type-2 diabetes had significantly lower HRV than those without it. Diabetics with chronic complications have even lower HRV.
The lower HRV observed in people with diabetes is likely related to many negative aspects of the disease, such as chronic stress, inflammation, and increased oxidative stress.
Perhaps unsurprisingly, low HRV is associated with adverse outcomes in diabetes. For example, people with diabetes and low HRV are at increased risk of coronary heart disease. Moreover, low HRV is an early marker of cardiac autonomic neuropathy, which can lead to heart disease, the number one cause of mortality in people with diabetes.
Sounds depressing, right?
Enter the Heart-Boosting Power of Slow Breathing
“When we breathe slowly at around 6 breaths per minute, we synchronize signals coming from our cardiovascular, respiratory, and autonomic nervous systems. ”
When we breathe slowly at around 6 breaths per minute, we synchronize signals coming from our cardiovascular, respiratory, and autonomic nervous systems.
To get a little more technical, we have baroreceptors monitoring blood pressure. They sense the changes in heart rate that accompany each breath. Then, they send their own signals to the heart.
For example, as blood pressure rises, they tell the heart to slow down. And as blood pressure falls, they tell the heart to speed up.
Here’s the issue: there’s about a 5-second lag for signals. Thus, they end up getting mingled together with the signals from the breath. One may be trying to increase heart rate while the other is trying to slow it down.
But when we breathe at about 6 breaths per minute, we synchronize these messages. (To breathe at 6 breaths per minute, we need about a 5-second inhale and 5-second exhale (or 4/6 also works). This matches the time lag from the baroreceptors.)
When the signals get synchronized, great things happen. Each breath amplifies heart rate oscillations, leading to greater HRV. This also balances the nervous system, making us calm and relaxed. If we do this regularly, it can significantly improve our quality of life.
Let’s break these down into a little more detail and look at 4 positive outcomes we get from slow breathing.
The 4 Key Benefits of Heart-Breath Synchronization for Diabetes
1. Improved Heart Rate Variability
This is the most potent effect. As mentioned, when we breathe slowly, we amplify the heart rate oscillations occurring with each breath. This increases HRV, a critical problem in diabetes.
One study published in Nature found that just 2 minutes of slow breathing at 6 breaths/min could bring the HRV of type-1 diabetics to levels of non-diabetic controls. (Side note: this was the paper that convinced me to start sharing this information. Nature is one of the most prestigious journals in the world. If they’re talking about slow breathing and diabetes, I realized my results weren’t so crazy after all.)
A long-term study of people with type 2 diabetes and ischemic heart disease found that one year of slow diaphragmatic breathing significantly increased HRV, and this wasn’t even at precisely 6 breaths per minute. Just slowing down the breath was enough to boost HRV.
And better HRV means better cardiovascular health and a longer life.
It also means more resiliency to diabetic stressors, but I’ll save that for another blog post.
“And better HRV means better cardiovascular health and a longer life.”
2. Efficiency and Blood Flow
When bodily messages come into harmony, it creates efficiency. Efficiency means your body doesn’t have to work as hard to complete its normal processes.
This efficiency also improves blood flow, a fundamental problem in diabetes. For example, the same 2-minute study mentioned above found that slow breathing also improved arterial function. Better arteries, more blood flow, and less chance of complications.
3. Reduced Blood Pressure
Slow breathing has consistently been shown to lower blood pressure. A 2019 meta-analysis found an average systolic blood pressure reduction of about 5 points from slow breathing for about 20 minutes daily.
The blood pressure-reducing effects of slow breathing have also been shown in diabetes. In a study of 65 type-2 diabetics with hypertension, slow breathing significantly reduced systolic and diastolic blood pressure.
These results are significant because Johns Hopkins Medical Center reports that people with diabetes are twice as likely to develop hypertension. It’s also estimated that anywhere from 40 to 80% of diabetics have hypertension. Moreover, a person with diabetes and hypertension is four times more likely to develop heart disease. For these reasons, preventing and treating hypertension is a chief concern in people with diabetes.
Slow breathing provides one complementary therapy for doing just that.
4. Less Stress & Anxiety
And lastly, we can’t discuss heart problems without discussing stress. We know when we’re stressed, we have chronic activation of the sympathetic (fight-or-flight) nervous system. This raises heart rate and blood pressure, adding extra strain on our hearts.
Fortunately, slow breathing is one of the fastest and most effective ways to alleviate stress. You’ve probably been told at some point in your life to “just take a deep breath.” It turns out there’s some solid science for this statement.
Slowing down the breath, especially with a longer exhalation, increases activity in the parasympathetic nervous system (rest-and-digest), reducing stress and increasing relaxation. Slow breathing also reduces activity in the amygdala (often referred to as the “fear center”), which also helps reduce stress.
Slow Breathing is a Superpower for Your Heart
To recap, slow breathing at about 6 breaths per minute is excellent for our hearts, especially if you have diabetes.
It harmonizes messages being sent from the cardiovascular and autonomic nervous systems. This leads to a ton of benefits, but here are 4 critical ones for diabetic heart health:
Improved heart rate variability
Increased efficiency and blood flow
Lower blood pressure
Less stress and anxiety
For these reasons, the paper published in Nature concluded:
“Slow breathing could be a simple beneficial intervention in diabetes.”
Simple and beneficial, indeed.
Start Improving Your Heart Health Today
I hope this article motivates you to start a slow breathing practice.
But, if you’d like some more help, you can check out the Breathing for Diabetes Online Course, which covers everything you need to get started.
I hope you’ll check it out, and if you have any questions about slow breathing in general, please email me at nick@thebreathingdiabetic. I always respond within 5 days (but usually ~2).