Listen to this Post as a 5-min Podcast:
"You cannot breathe your way out of a Big Mac."
But apparently, slow breathing might help it taste better (see #3 below).
Ok, let’s get to it. Here are 4 thoughts, 1 quote, and 1 answer for the week. Enjoy!
4 THOUGHTS
1. Is There Really “Dysfunctional” Breathing?
"Breathing is one of the body’s critical functions. When its fundamental processes break down, the body will compensate, calling on structures such as the core muscles to help maintain respiration."
– Patrick McKeown, The Breathing Cure (pg. 152)
Breathing is the body’s most critical function. So as Patrick tells us, even if we do it incorrectly, the body will compensate by activating whatever muscles are needed to keep it going. Breathing takes precedence over everything.
So, we might say that breathing will always remain "functional" in that it will always do its main task of keeping us alive. But, it might be severely inefficient.
Thus, "dysfunctional" breathing is really just inefficient breathing.
This gives us two options. We can develop optimal breathing, which uses the nose and activates the diaphragm. Or, we can ignore our breathing and let the body compensate on its own, usually in ways that are detrimental to our health.
I say we choose option 1.
2. Diabetes, Oxidative Stress, and Slow Breathing
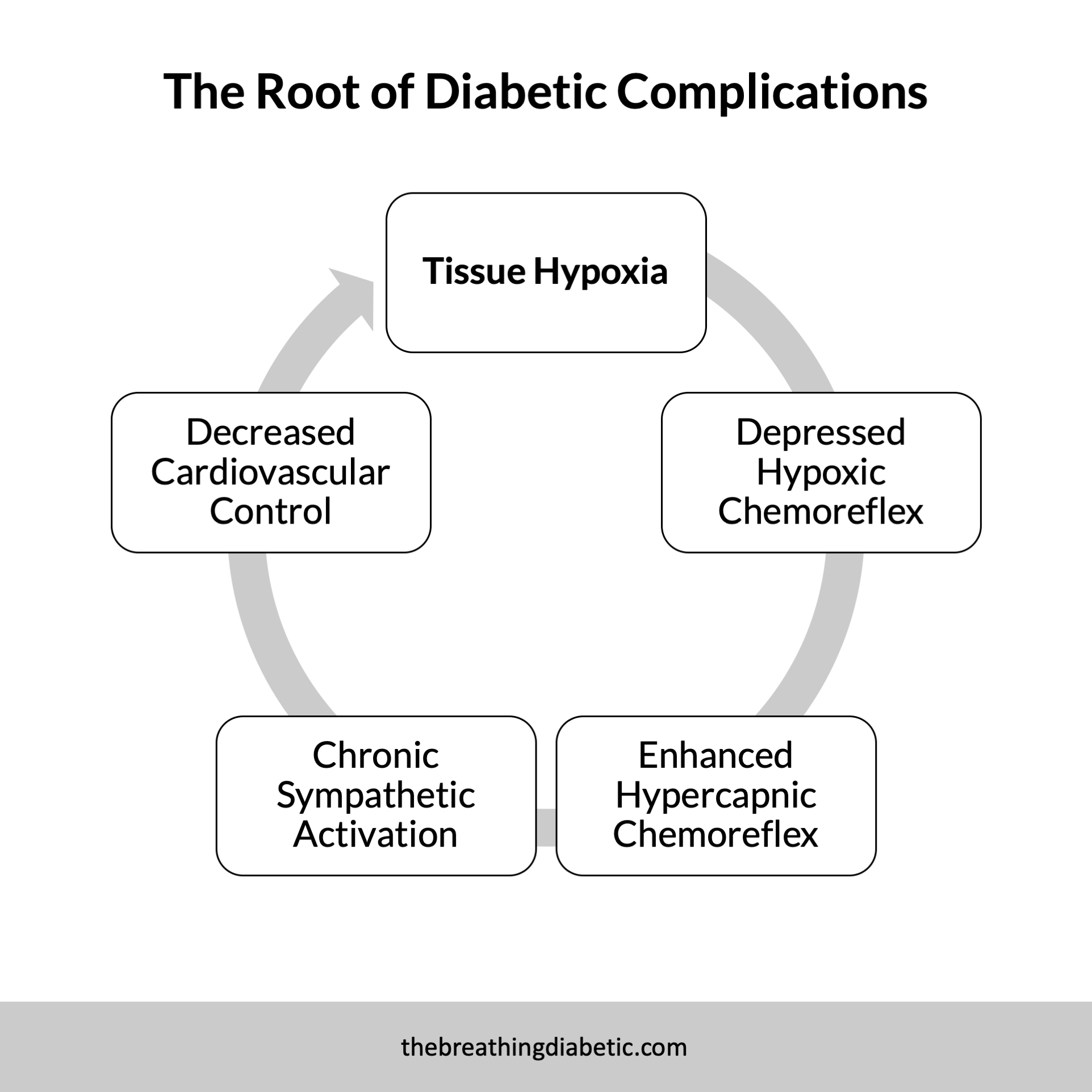
High blood sugars generate free radicals. These excess free radicals deplete antioxidants and ultimately cause oxidative stress. This negative feedback loop has been described as the "single unifying mechanism for diabetic complications."
To combat this, people with diabetes would ideally find a way to both reduce free radical production and increase antioxidant defenses. Slow breathing provides a natural and effective method of doing just this.
For example, slow diaphragmatic breathing reduces post-meal oxidative stress. It also reduces oxidative stress associated with intense, long-duration exercise. The hallmark paper on slow breathing & diabetes published in Nature even said:
"…our results lead to the hypothesis that slow breathing may exert some antioxidant effect, possibly via parasympathetic stimulation."
Taken together, slow breathing appears to be a simple and effective way to help with oxidative stress in diabetes. Quite amazing.
3. Apparently Slow Breathing Makes Food Taste Better
"Smooth, relatively slow breathing maximises delivery of the particles to the nose. Food smells and tastes better if you take your time."
This was a fun read from Vice. At first, I thought it seemed a bit silly. But the study was originally published in PNAS, so maybe there’s something to it?
If we pair this advice with Ch. 7 of Breath, we might say that to enjoy a meal, breathe slowly and chew more. I’m constantly working on the chew more part…
Enjoy!
4. Take the Nose, Take the Life
"Ancient Egyptian cultures also recognized the importance of the breath, the evidence of which we see today in the many ancient statues that had their noses broken off but otherwise were left untouched. This defacement was no accident, but a deliberate act by conquering groups to take the life, in this case the breath of life, away from these icons."
- Michael J. Stephen, MD, Breath Taking
This is on the first page of the book. Although Dr. Stephen never mentions the power of the nose again, it’s a rather remarkable statement that emphasizes just how important the breath (and nose) were to ancient cultures.
1 QUOTE
"Civilized man may properly be said to be an open mouthed animal; a wild man is not."
- George Catlin, The Breath of Life (1864)
1 ANSWER
(This one blows my mind…)
Answer: The inner surface of this organ has as many hair follicles as your head.
…
(Cue the Jeopardy! music.)
…
Question: What is your nose?
In good breath,
Nick
P.S. He was the dog.