Listen Instead of Reading
The way you breathe might affect your insulin sensitivity. And the way you walk definitely affects your ability to withstand discomfort.
Let’s find out how…
4 Thoughts
1. Longer Exhalations are Naturally Relaxing
“It's helpful to extend your exhalations because the ‘rest and digest’ parasympathetic nervous system handles exhaling while also slowing your heart rate. So, longer exhalations are naturally relaxing.”
- Rick Hanson, Ph.D., Neurodharma
Just a friendly reminder that extending the exhalation is one of the fastest ways to naturally relax. That is all : )
***
Related: Longer Exhalations Are an Easy Way to Hack Your Vagus Nerve
Related: BBC: Why slowing your breathing helps you relax
2. How Breathing Might Help with Insulin Sensitivity
“These observations demonstrate that hypoxia rapidly regulated the inhibition of the insulin signaling pathway […] During reoxygenation, the ability of insulin to stimulate phosphorylation of insulin receptor and signaling proteins was restored after 45 min.”
– Hypoxia Decreases Insulin Signaling Pathways in Adipocytes
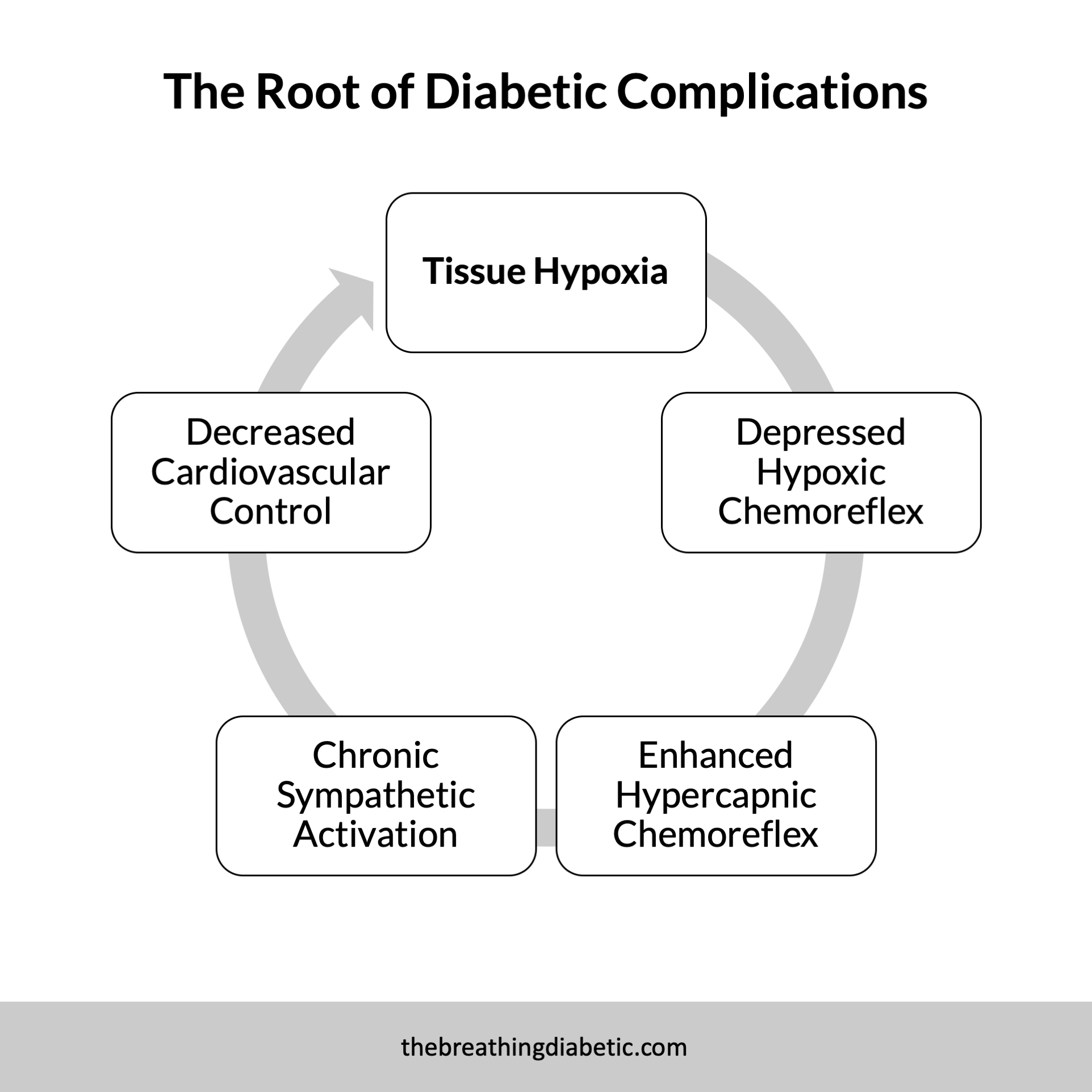
Insulin resistance is a critical factor in diabetes and overall metabolic health. In this paper, we learn that low tissue oxygen (hypoxia) can trigger insulin resistance. Encouragingly, however, reoxygenation restored it.
This is one reason why optimal breathing is so essential for metabolic health, especially for people with diabetes. By practicing slow nasal breathing, we increase our blood and tissue oxygenation. This could potentially maintain, or even restore, insulin sensitivity.
Of course, there is no research showing that slow nasal breathing does this—no one is going to fund that study : ) But, given what we know about slow breathing, tissue oxygenation, and blood flow, it seems reasonable to hypothesize that it would help. I know have certainly noticed a difference.
***
Related: The Lesser-Known Benefits of Nasal Breathing, Designed for Diabetes
3. “Role of respiration in mind-body practices: concepts from contemporary science and traditional yoga texts”
“Traditional yoga texts also suggest a solution for the imbalance in prana, through slow, deep breathing. … The beneficial effects of deep breathing are supported by contemporary science.”
I’ve shared a quote from this paper before, but if you haven’t read the full thing, it’s well worth it. It describes how modern science supports ancient yogic breathing, for example, how “Conventional physiology has found benefits of deep breathing supporting the importance given to regulating the breath in yoga.”
Another interesting idea they mention is that breathing “acts as both a top-down and bottom-up mind-body practice.” It makes perfect sense, but I hadn’t thought about it that way.
Ancient Yogic Wisdom + Modern Science = A Fantastic Read
Enjoy!
4. Finding Comfort in Breathwalking
“To take my mind off the discomfort, I settle into a respiratory rhythm. I take one step as I breathe in, then two steps as I breathe out. One step breathing in, two steps breathing out. Over and over, focusing only on the breath.”
- Michael Easter, The Comfort Crisis
Easter spent more than a month in a remote region of Alaska. And this book that came out of it is incredible—a perfect blend of science and storytelling.
Of course, this part stood out to me : )
Easter is making a ridiculous walk back to camp with a ton of weight. He naturally settles into his breath, and this gives him comfort and endurance.
As he puts it, “There's science behind this. Brazilian researchers found that people who are able to detach from their emotions during exercise, for example, not thinking about or putting a negative valence on their burning legs and lungs, almost always perform better.”
So aside from the mechanics and oxygenation, here’s another way in which breathwalking can be beneficial. It helps you detach from your emotions. As Easter tells us, you’ll “almost always perform better.” Sounds good to me.
***
Related: Breathwalking with Gandhi
1 Quote
“He let me see that, because the breath is so unassuming, I had been undervaluing it. I was looking for a complicated path to enlightenment, when this simple one was right before me.”
- Larry Rosenberg, Breath by Breath
1 Answer
Category: Hypoxia
Answer: A blood oxygen saturation below approximately this value is considered hypoxic.
…
(Cue the Jeopardy! music.)
…
Question: What is 90%?
P.S. Different places give slightly different numbers…sometimes it’s 94%, sometimes 92%.
In good breath,
Nick Heath, T1D, PhD
“Breathing is the compound interest of health & wellness.”
P.S. What if?
Sign Up For The Breathing 411
Each Monday, I curate and synthesize information from scientific journals, books, articles, and podcasts to share 4 thoughts, 1 quote, and 1 answer (like "Jeopardy!") related to breathing. It’s a fun way to learn something new each week.