Principle 1: Breathe Through Your Nose
This is the simplest and most effective way to improve your breathing. Start breathing through your nose 24/7 (especially during sleep).
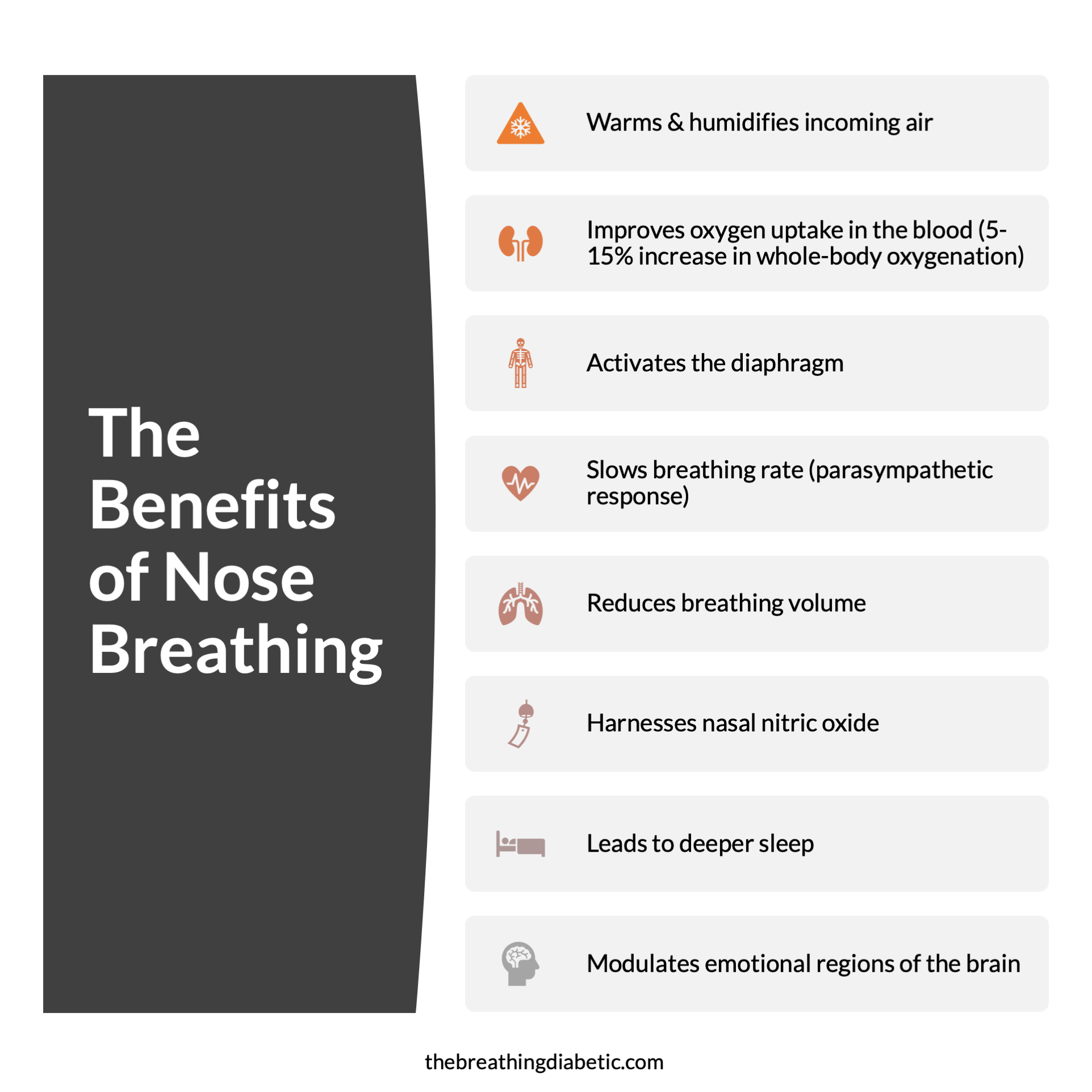
The Benefits of Nose Breathing
The nose warms and humidifies the incoming air, improves gas exchange in the lungs, naturally activates the diaphragm, and slows down your breathing rate to activate the parasympathetic nervous system (see Principle 2). Studies have shown that simply switching from mouth breathing to nose breathing can increase whole-body oxygenation by 10%.
The Secret Gas Behind the Benefits of Nasal Breathing
Much of the benefits described above actually come from nitric oxide (NO). Nitric oxide is continuously produced in the paranasal sinuses. When you breathe through your nose, NO is carried into the lungs with each breath. Because NO is a potent vasodilator (hence its use in Viagra), it redistributes blood flow in the lungs to increase gas exchange. This results in better blood oxygenation.
Nitric oxide is also antimicrobial and antiviral, meaning it helps protect you from pathogens in the air you breathe. Moreover, NO enhances the functioning of the cilia that line the airways. These tiny hairs oscillate back and forth to push inhaled particles and pathogens out of the airways to be swallowed with the mucus or excreted by sneezing or coughing. They are your lungs’ first line of defense against dirty air, and NO helps them work better.
If that wasn’t enough, nasal NO also helps warm incoming air. Because it is a powerful vasodilator, NO acts to increase blood flow in the nasal airways, which increases temperature. As air travels through, it extracts that heat so that it is better conditioned for the lungs.
Carbon Dioxide is Not Waste
One misconception about breathing is that carbon dioxide (CO2) is simply a waste product that our body needs gets rid of. Nothing could be farther from the truth.
Carbon dioxide plays a crucial role in getting oxygen into our tissues and organs. It loosens the bond between hemoglobin and oxygen (known as the Bohr effect), allowing oxygen to more readily be released into organs and tissues that need it.
It’s not about breathing more oxygen. It’s about getting that oxygen to the cells and tissues that need it.
You can think of CO2 as being to oxygen what insulin is to glucose. You need insulin to get glucose out of your blood and into your tissues and organs. You need CO2 to get oxygen out of your blood into your tissues and organs.
Breathing through the nose naturally reduces breathing volume, helping retain more carbon dioxide. This leads to better oxygenation of the cells, tissues, muscles, and organs. This is critical to diabetes because tissue hypoxia might be the root cause of diabetic complications.
It seems counter-intuitive, but with breathing, less is more.
Your Brain on Nasal Breathing
When you breathe through your nose, it “lights up” broad regions of the olfactory bulb, a portion of your brain typically associated with smell.
However, the airflow itself, rather than odor, causes much broader activation of the olfactory bulb. A simple Wiki search will give you the significance of these findings:
“It [the olfactory bulb] sends olfactory information to be further processed in the amygdala, the orbitofrontal cortex (OFC) and the hippocampus where it plays a role in emotion, memory and learning.”
A study also showed that nasal breathing synchronizes brain wave oscillations in the piriform cortex, amygdala, and hippocampus. This led to improved cognitive function when compared to mouth breathing.
These findings of how nasal breathing impacts the brain helps us understand why it can have profound effects on emotion and memory.
Nasal Breathing: The Key to Deeper Sleep
A couple that tapes together, stays together.
Of all the things I’ve tried, taping my mouth at night has had the most significant positive impact on my health. I would argue that this entire website and all of my research is the result of the energy I gained from taping at night. Of course, not everyone will respond in the same way I did. But, taping requires minimal effort for the health benefits it provides.
As we’ve learned so far, there are many benefits of breathing through your nose. An important one during sleep is that it helps slow down your breath, which will help you shift from a sympathetic state to a parasympathetic state. This shift is especially important for people with diabetes who exhibit less parasympathetic tone at night than non-diabetics.
Taping our mouth helps us increase parasympathetic tone and enjoy better sleep.
Receptors in your nose also act to maintain rhythmic breathing during sleep, which may help explain why nose breathing reduces the risk of obstructive sleep apnea. Yes, it sounds and looks ridiculous to tape your mouth shut at night. But, taping will result in deeper sleep, more energy and focus during the day, less snoring, and will reduce dry mouth and bad breath in the morning.
Finally, we know that inadequate sleep causes insulin resistance. By getting deeper, more restorative sleep, you will improve insulin sensitivity. You might even see dramatic improvements in your morning blood sugars (like I did) from this one simple change. Try it for a few nights and see how you feel.
“While asleep, shut your mouth and save your brain.” - Sleep (1983)
Practice Principle 1
Actionable Steps
Notice when you are mouth breathing and consciously switch to the nose.
Breathe through your nose during physical exercise — This can be difficult at first, but will lead to long-term improvements in oxygen utilization.
Use tape to keep your mouth closed at night (see details below).
Taping at Night
I use 3M micropore paper tape that I purchase on Amazon. My wife uses Lipsealtape (now Simply Breathe) because it does not dry out her lips and it is easy to remove in the morning.
If you are nervous about taping, try it out during the day until you become comfortable with it.
Lastly, you’ll probably notice that the tape does not stay on an entire night at first. This is normal. As you get used to nasal breathing at night, the tape will gradually stay on longer and longer, until you keep it on all night.
WARNING: Don’t tape your mouth shut if you’re sick, after drinking excessive amounts of alcohol, if you are taking sedative medications, if you have difficulty using the tape during the day, or if you have trouble breathing through your nose in general (consult your physician in that case).
If you enjoyed this page, consider signing up for
The Breathing 4.1.1. Newsletter.
Each Monday I share 4 thoughts, 1 quote, and 1 answer (think "Jeopardy") related to breathing. This is the best place to get all of the latest information from the site. View previous versions here.